The Role of the Gut Microbiome in Rosacea
The microbes living within our gut don’t just help us to digest food, they also influence the way our immune system functions, our metabolism, and even the health of our skin. When the gut microbiome is balanced, this helps to keep inflammation under control. But when it becomes disrupted, this can set off a cascade of immune and inflammatory responses that affect all areas of the body, including the skin. Disruptions in the gut microbiome may play a role in triggering rosacea. Notably, studies have found higher rates of gut disorders such as small intestinal bacterial overgrowth (SIBO), irritable bowel syndrome, and even Helicobacter pylori infections in people with rosacea.,, These associations suggest that an imbalanced gut may set the stage for skin inflammation, either by increasing systemic inflammation or by altering how the immune system responds to environmental triggers.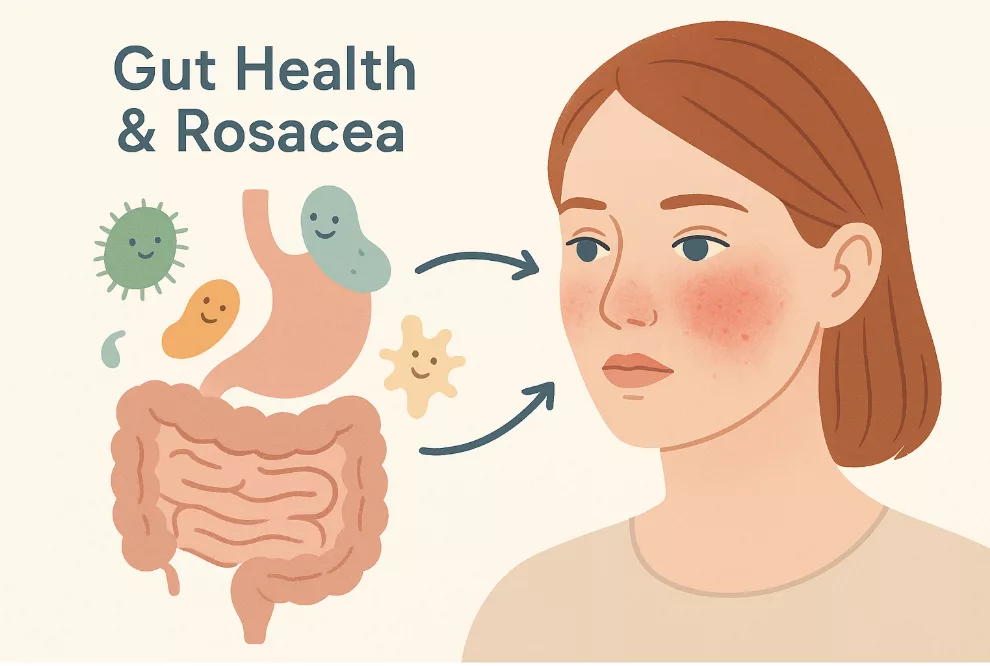 Studies have also shown that rosacea patients often exhibit significant alterations in gut microbial diversity and composition. For example, one study showed that people with rosacea had lower microbial richness and diversity and distinct beta diversity patterns. Furthermore, beneficial bacteria such as Faecalibacterium prausnitzii, Lachnospiraceae ND3007 group, and Ruminococcaceae were significantly reduced, while Oscillobacter, Flavonifractor plautii, and Ruminococcaceae UBA 1819 were significantly increased. Meanwhile, in a separate case-control study, rosacea patients also showed reduced abundance of Lactobacillus, Megasphaerae, Acidaminococcus, Haemophilus, Roseburia, Clostridium, and Citrobacter, alongside enrichment of Rhabdochlamydia, CF231, Bifidobacterium, Sarcina, and Ruminococcus. These microbial changes were linked to alterations in metabolic genes involved in colonic sulfur metabolism and cobalamin transport, providing possible mechanisms through which gut microbes could influence skin inflammation in rosacea.
Emerging evidence also points to a causal role of gut bacteria in the development of rosacea. Specifically, a Mendelian randomization study found that two bacterial groups, Actinobacteria and Butyrivibrio, appeared to protect against rosacea, while fourteen other gut bacteria were linked to different rosacea types.
These findings highlight how shifts in gut microbial composition and function may not only contribute to the development of rosacea but also trigger flare-ups, linking underlying dysbiosis to both disease onset and episodic inflammation. This paves the way to explore exactly how gut imbalance can drive rosacea episodes and interact with known triggers.
Studies have also shown that rosacea patients often exhibit significant alterations in gut microbial diversity and composition. For example, one study showed that people with rosacea had lower microbial richness and diversity and distinct beta diversity patterns. Furthermore, beneficial bacteria such as Faecalibacterium prausnitzii, Lachnospiraceae ND3007 group, and Ruminococcaceae were significantly reduced, while Oscillobacter, Flavonifractor plautii, and Ruminococcaceae UBA 1819 were significantly increased. Meanwhile, in a separate case-control study, rosacea patients also showed reduced abundance of Lactobacillus, Megasphaerae, Acidaminococcus, Haemophilus, Roseburia, Clostridium, and Citrobacter, alongside enrichment of Rhabdochlamydia, CF231, Bifidobacterium, Sarcina, and Ruminococcus. These microbial changes were linked to alterations in metabolic genes involved in colonic sulfur metabolism and cobalamin transport, providing possible mechanisms through which gut microbes could influence skin inflammation in rosacea.
Emerging evidence also points to a causal role of gut bacteria in the development of rosacea. Specifically, a Mendelian randomization study found that two bacterial groups, Actinobacteria and Butyrivibrio, appeared to protect against rosacea, while fourteen other gut bacteria were linked to different rosacea types.
These findings highlight how shifts in gut microbial composition and function may not only contribute to the development of rosacea but also trigger flare-ups, linking underlying dysbiosis to both disease onset and episodic inflammation. This paves the way to explore exactly how gut imbalance can drive rosacea episodes and interact with known triggers.
Gut Dysbiosis: How Imbalance May Drive Flare-Ups
 Shifts in gut microbial composition can actively influence when and how rosacea flares, by altering metabolite production (such as the production of short-chain fatty acids), which circulate systemically and can affect immune responses, vascular reactivity, and skin barrier function. These changes may help explain why triggers such as diet, stress, alcohol, or antibiotics can suddenly worsen symptoms, turning a previously controlled condition into a full-blown flare-up.
It’s important to note that dysbiosis patterns can vary between individuals, meaning the specific bacterial changes driving flare-ups may differ from person to person. Understanding these individual differences is key to exploring targeted strategies for managing rosacea and preventing future flare-ups.
Shifts in gut microbial composition can actively influence when and how rosacea flares, by altering metabolite production (such as the production of short-chain fatty acids), which circulate systemically and can affect immune responses, vascular reactivity, and skin barrier function. These changes may help explain why triggers such as diet, stress, alcohol, or antibiotics can suddenly worsen symptoms, turning a previously controlled condition into a full-blown flare-up.
It’s important to note that dysbiosis patterns can vary between individuals, meaning the specific bacterial changes driving flare-ups may differ from person to person. Understanding these individual differences is key to exploring targeted strategies for managing rosacea and preventing future flare-ups.
Personalized Treatment Strategies for Rosacea
As there will always be considerable variability in gut microbiome composition and specific disease triggers between patients, a one-size-fits-all approach to rosacea treatment is often insufficient. With personalized treatment approaches, the aim is to figure out what imbalances are driving symptoms in each patient, so that interventions such as diet changes, lifestyle tweaks like reducing stress or alcohol intake, or probiotics, can be tailored for the best results. Evidence is growing that modulating the gut microbiome can make a real difference. For example, in a clinical trial, patients with papular-pustular rosacea who took E. coli Nissle alongside a vegetarian diet and standard topical therapy saw significant improvement in their symptoms, compared to those who received diet and topicals alone. Improvements included better skin, normalized stools, and a shift towards protective gut bacteria. Supporting this approach, a recent mouse study tested two probiotic strains, Ligilactobacillus salivarius 23-006 and Lacticaseibacillus paracasei 23-008, for their effects on rosacea-like skin inflammation. The combination of these strains reduced skin lesions and inflammation, improved gut microbiota balance, and strengthened the intestinal barrier. These findings highlight how targeting the gut microbiome could be a practical strategy to manage rosacea.How Enbiosis Supports Microbiome Balance
 At Enbiosis, we use advanced AI and whole-genome sequencing techniques to empower patients to take a personalized approach to their gut health and skin wellness. By assessing individual microbiome profiles, we can identify imbalances that may be driving skin conditions, such as rosacea.
Based on the comprehensive data that we collect, we provide actionable and personalized food scores to highlight which foods best support beneficial microbes and correct missing microbial functions. We also offer precision-matched probiotic and prebiotic recommendations, designed to target specific imbalances, increase microbial diversity, and help alleviate symptoms.
By combining these insights and interventions, Enbiosis makes personalized gut microbiome care practical, effective, and tailored to each individual’s needs. Contact us today to find out more.
At Enbiosis, we use advanced AI and whole-genome sequencing techniques to empower patients to take a personalized approach to their gut health and skin wellness. By assessing individual microbiome profiles, we can identify imbalances that may be driving skin conditions, such as rosacea.
Based on the comprehensive data that we collect, we provide actionable and personalized food scores to highlight which foods best support beneficial microbes and correct missing microbial functions. We also offer precision-matched probiotic and prebiotic recommendations, designed to target specific imbalances, increase microbial diversity, and help alleviate symptoms.
By combining these insights and interventions, Enbiosis makes personalized gut microbiome care practical, effective, and tailored to each individual’s needs. Contact us today to find out more.
References:
• National Rosacea Society. (2024, May 23). New study estimates rosacea’s worldwide prevalence. Rosacea.org. Retrieved September 2, 2025, from https://www.rosacea.org/blog/2024/may/new-study-estimates-rosaceas-worldwide-prevalence
• Frydrych, Z. L., Chwarścianek, N., Błaszak, K., & Czajkowski, R. (2023). The potential role of Helicobacter pylori and other gut dysbiosis factors in the development of rosacea. Forum Dermatologicum, 9(4), 138–142.
• Drago, F., et al. (2016). The role of small intestinal bacterial overgrowth in rosacea: A 3-year follow-up. Journal of the American Academy of Dermatology, 75(3), e113–e115.
• Wang, F. Y., & Chi, C. C. (2021). Rosacea, Germs, and Bowels: A Review on Gastrointestinal Comorbidities and Gut-Skin Axis of Rosacea. Advances in Therapy, 38(3), 1415–1424.
• Guertler, A., Hering, P., Pacífico, C., Gasche, N., Sladek, B., Irimi, M., French, L. E., M., B., & Reinholz, M. (2024). Characteristics of Gut Microbiota in Rosacea Patients—A Cross-Sectional, Controlled Pilot Study. Life, 14(5), 585.
• Li, J., Yang, F., Liu, Y., & Jiang, X. (2024). Causal relationship between gut microbiota and rosacea: A two-sample Mendelian randomization study. Frontiers in Medicine, 11, Article 1322685.
• Qi, X., Xiao, Y., Zhang, X., Zhu, Z., Zhang, H., Wei, J., Zhao, Z., Li, J., & Chen, T. (2024). Probiotics suppress LL37 generated rosacea-like skin inflammation by modulating the TLR2/MyD88/NF-κB signaling pathway. Food & Function, 15(17), 8916–8934.