Table of Contents
The Hidden Link Between PCOS and Gut Health
Polycystic ovary syndrome (PCOS) is a common hormonal imbalance disorder which affects around 6-13% of reproductive-age women around the world (1) It is thought to be caused by a combination of genetic and environmental factors. However, there’s another key player that’s often overlooked—the gut microbiome.
Emerging evidence suggests that imbalances in our gut microbes may be fueling PCOS symptoms. So, let’s explore what PCOS is, how the microbiome affects it, and whether gut-focused interventions could offer a new approach for treatment.
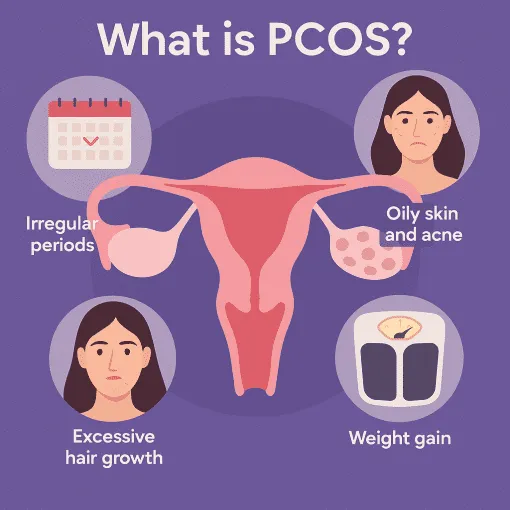
What is PCOS?
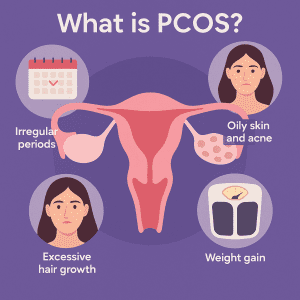 PCOS affects the functioning of the ovaries, resulting in an imbalance of reproductive hormones. Individuals with PCOS typically develop many small, fluid-filled sacs called follicles across their ovaries. These follicles can affect the release of eggs and contribute to high androgen levels, which are hormones that play a significant role in male development.
PCOS affects the functioning of the ovaries, resulting in an imbalance of reproductive hormones. Individuals with PCOS typically develop many small, fluid-filled sacs called follicles across their ovaries. These follicles can affect the release of eggs and contribute to high androgen levels, which are hormones that play a significant role in male development.
Symptoms of PCOS include irregular or missed periods, fertility problems, weight gain, excessive hair growth on the face, chest and back, oily skin and acne. PCOS may also be associated with a higher risk of certain other health conditions, including cardiovascular disease, infertility and type 2 diabetes.
While the exact cause of PCOS isn’t yet fully understood, genetics, insulin resistance, and inflammation are believed to be key drivers of the condition. Many individuals with PCOS have higher insulin levels, which can increase androgen production and contribute to symptoms. Beyond hormones, emerging research suggests that gut microbiome imbalances may also play a role in PCOS, offering a potential link between metabolic dysfunction and the disorder.
How Does the Gut Microbiome Influence PCOS?
As our understanding evolves, research shows that our gut microbes play a role in the balance of hormones within our bodies and also in the development of systemic inflammation, both of which are key factors in PCOS. This has prompted researchers to explore how gut dysbiosis directly impacts these metabolic and endocrine aspects in women with PCOS.
Firstly, one of the key ways an imbalanced gut microbiome can impact ovarian function is through its role in insulin resistance, which is present in a significant number of women with the condition. When the gut microbiome is out of balance, this can interfere with the body’s ability to process glucose efficiently, leading to higher insulin levels and worsening PCOS symptoms (2)
Secondly, a dysbiotic gut microbiome can also contribute to chronic low-grade inflammation, which is often seen in women with PCOS. This is because the gut is closely linked with the body’s immune system and regulation of inflammatory responses. Structural components of certain gut bacteria can initiate widespread inflammatory responses, while some metabolic by-products of bacterial activity can counteract inflammation and promote anti-inflammatory effects.
Finally, the microbes within our gut can also directly impact hormone levels within the body, particularly those that are involved in our reproductive health. For instance, many gut microbes produce β-glucuronidase, an enzyme that prevents the inactivation of estrogen, helping to maintain active estrogen levels in the body. They can also influence levels of progesterone and androgens, contributing to a balanced hormonal environment (3)
Gut Microbiome Changes in PCOS
 Building on these mechanisms, studies have revealed that women with PCOS often exhibit lower microbial diversity and shifts in specific gut bacterial populations. This may contribute to the metabolic and hormonal imbalances seen with this condition. Specifically, PCOS patients have been shown to have decreased alpha and beta diversity, indicating a less diverse and imbalanced gut microbiome (4)
Building on these mechanisms, studies have revealed that women with PCOS often exhibit lower microbial diversity and shifts in specific gut bacterial populations. This may contribute to the metabolic and hormonal imbalances seen with this condition. Specifically, PCOS patients have been shown to have decreased alpha and beta diversity, indicating a less diverse and imbalanced gut microbiome (4)
In a recently published review of fourteen research studies, specific bacterial taxa were shown to be altered in PCOS patients compared to healthy controls. Within these studies, women with PCOS had a higher abundance of Fusobacterium, Ruminococcus gnavus, and Escherichia-Shigella and lower levels of Dysosmobacter, Schaedlerella, and Clostridiisalibacter. Interestingly, gut microbial differences varied regionally and also depended on testosterone levels, with patients with higher testosterone levels having greater levels of Prevotella, Blautia, Dialister, Ruminococcus_torques_group and UCG-002 and lower levels of Alistipes, Dysosmobacter, Phocaeicola and Faecalibacterium (5)
Likewise, a pilot study showed that, while dominant bacterial groups remained relatively stable, PCOS patients had changes in levels of some less common bacteria. Notably, levels of Tenericutes and the S24-7 family (from Bacteriodetes) were lower in PCOS patients and this was associated with reproductive parameters. In the same study, PCOS patients also showed changes in some markers of gut barrier integrity.
Significantly, women with PCOS who also have insulin resistance have been shown to have a different gut microbiome profile compared to healthy women and those with PCOS alone. In particular, women with PCOS and insulin resistance have more Enterococcus bacteria, which may contribute to insulin resistance by altering gut metabolism (6)
A notable finding in women with both PCOS and mood disorders is a decreased abundance of Butyricicoccus. This beneficial gut bacteria is involved in the production of the short-chain fatty acid, butyrate, which plays a key role in maintaining gut barrier integrity and regulating inflammation. Thus, reduced levels of Butyricicoccus may contribute to heightened neuroinflammation, potentially exacerbating mood disorders commonly seen in PCOS patients (7)
Meanwhile, increased levels of Sutterella in PCOS patients have been linked to metabolic factors, including glucose metabolism, obesity and gut barrier integrity, suggesting a potential role in driving insulin resistance and systemic inflammation in affected individuals.8
Can Improving Gut Health Help to Manage PCOS?
Given the significant role that our gut microbiome plays in regulating both metabolic and hormonal balance in PCOS, it raises the question: can improving our gut health offer a viable strategy for managing PCOS symptoms?
Recent studies highlight that dietary changes may positively impact PCOS symptoms, potentially improving insulin resistance and fertility issues. However, a personalized approach may be most effective here, as gut microbial profiles can vary significantly from patient to patient. As we discussed earlier, individuals with PCOS exhibit diverse microbial imbalances, with variations in patients exhibiting insulin resistance and co-occurring mood disorders. Therefore, tailored dietary modifications that address these specific imbalances are likely to yield the most beneficial outcomes (9)
How Enbiosis Uses the Microbiome to Support PCOS
At Enbiosis, we take a personalized approach to managing PCOS by offering advanced AI-driven microbiome analysis to allow us to understand each patient’s unique gut microbial profile. The results from this comprehensive analysis then allow us to offer tailored dietary recommendations which are designed to address specific imbalances and improve overall metabolic and hormonal health.
All of our recommendations are data-driven and backed by science, helping us to optimize health outcomes for individuals with PCOS. To find out more about our services, visit our website or contact us today.
Contact UsReferences:
1) World Health Organization. (2025, February 7). Polycystic ovary syndrome. https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
2)Yang, L., Zhou, W., Wu, S., Tang, L., Wang, W., Zhou, Y., Li, W., Huang, F., He, Y., & Zhou, W. (2021). Intestinal Flora is a Key Factor in Insulin Resistance and Contributes to the Development of Polycystic Ovary Syndrome. Endocrinology, 162(10), bqab118.
3) He, S., Li, H., Yu, Z., Zhang, F., Liang, S., Liu, H., Chen, H., & Lü, M. (2021). The Gut Microbiome and Sex Hormone-Related Diseases. Frontiers in Microbiology, 12, 711137.
4) Gu, Y., Zhou, G., Zhou, F., Li, Y., Wu, Q., He, H., Zhang, Y., Ma, C., Ding, J., & Hua, K. (2022). Gut and Vaginal Microbiomes in PCOS: Implications for Women’s Health. Frontiers in Endocrinology, 13, 808508.
5) Yang, Y., et al. (2023). Gut microbiota in women with polycystic ovary syndrome: An individual-based analysis of publicly available data. eClinicalMedicine, 77.
6) Lindheim, L., Bashir, M., Münzker, J., Trummer, C., Zachhuber, V., Leber, B., Horvath, A., Pieber, T. R., Gorkiewicz, G., Stadlbauer, V., & Obermayer-Pietsch, B. (2017). Alterations in Gut Microbiome Composition and Barrier Function Are Associated with Reproductive and Metabolic Defects in Women with Polycystic Ovary Syndrome (PCOS): A Pilot Study. PLOS ONE, 12(1), e0168390.
7) He, F., & Li, Y. (2021). The gut microbial composition in polycystic ovary syndrome with insulin resistance: Findings from a normal-weight population. Journal of Ovarian Research, 14(50).
8) Lee, S., Tejesvi, M. V., Hurskainen, E., Aasmets, O., Franks, S., Tapanainen, J. S., Ruuska, T. S., Altmäe, S., Org, E., Salumets, A., Arffman, R. K., & Piltonen, T. T. (2024). Gut bacteriome and mood disorders in women with PCOS. Human Reproduction, 39(6), 1291-1302.
9) Kotusiewicz, W., Siekierko, N., Żołnierek, M., Lubczyńska, Z., Popravko, Y., Świętochowski, J., Lewandowski, M., & Bienia, G. (2023). Impact of various dietary interventions on the reduction of symptoms in polycystic ovary syndrome (PCOS). Journal of Education, Health and Sport. Online, 13(4), 311–318
10) Zhang, X., Zheng, Y., Guo, Y., & Lai, Z. (2019). The Effect of Low Carbohydrate Diet on Polycystic Ovary Syndrome: A Meta-Analysis of Randomized Controlled Trials. International Journal of Endocrinology, 2019(1), 4386401. https://doi.org/10.1155/2019/4386401
11) Shang, Y., Zhou, H., He, R., & Lu, W. (2021). Dietary Modification for Reproductive Health in Women With Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Frontiers in Endocrinology, 12, 735954.