Table of Contents
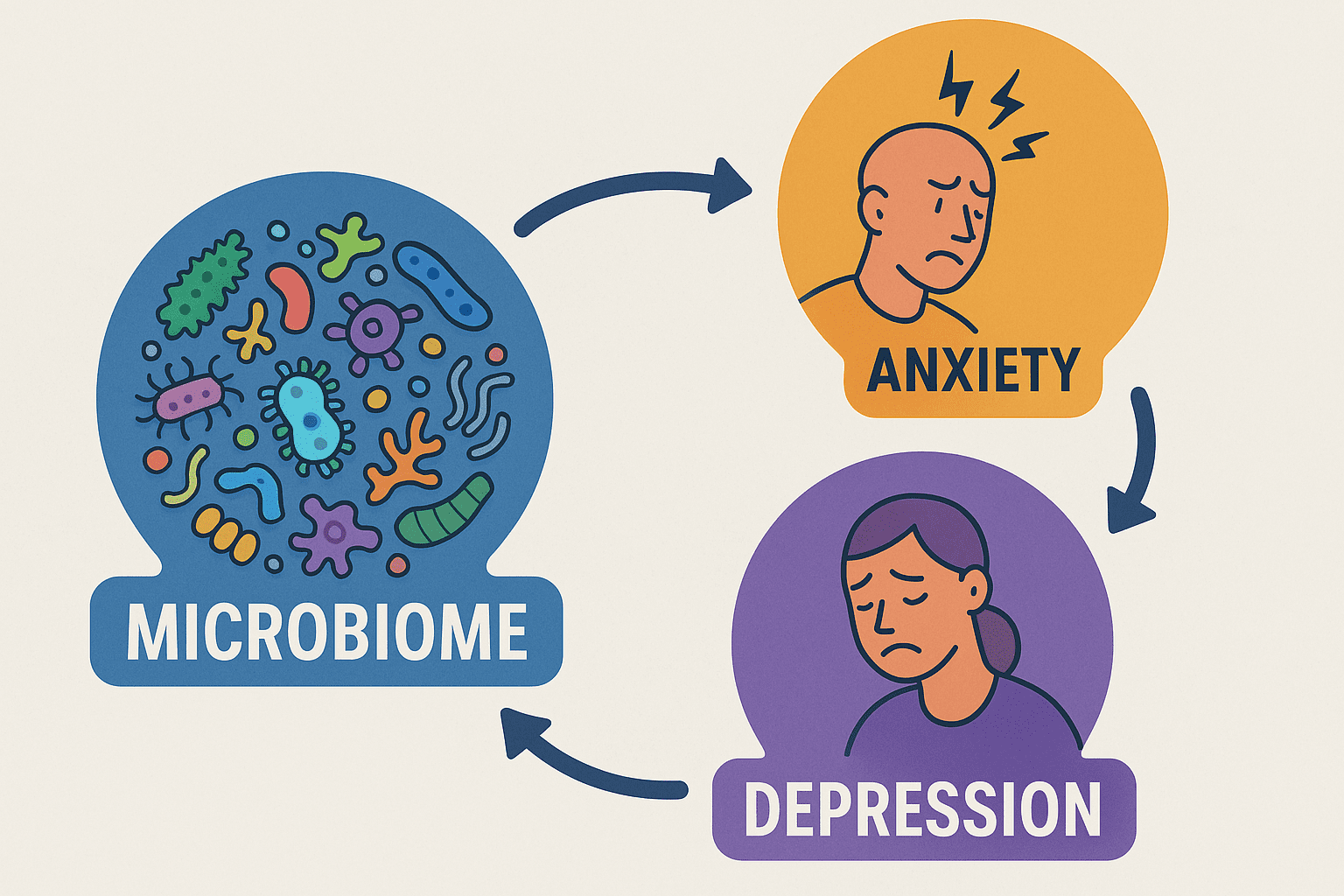
Anxiety and Depression May Begin in the Gut: Discover the Microbiome-Mind Connection
For years, mental health research has focused primarily on the brain, but emerging evidence suggests that depression and anxiety may have roots in an unexpected place—the gut. These common mental health conditions affect between 4-5% of the global population (1,2) and the gut may hold the key to new treatments. Join us as we learn more about this exciting connection.
What Are The Symptoms of Anxiety and Depression?
While anxiety and depression are two distinct mental health conditions, they can often co-occur and significantly impact an individual’s quality of life. Anxiety typically manifests as excessive worry, difficulty concentrating and restlessness. Those affected may also experience physical symptoms, such as an increased heart rate or trouble sleeping. Meanwhile, depression is generally characterized by persistent sadness or low mood, loss of interest in everyday activities, and feelings of hopelessness.
How Does the Gut Microbiome Shape Mental Health?
While it may sound surprising, the microorganisms living within our gut actually play a key role in shaping our mental health. Our gut microbes, collectively known as the gut microbiome, communicate with the brain via a complex bi-directional process which links the central and enteric nervous systems.
An essential part of this gut-brain communication involves the production of neurotransmitters, which are chemical messengers produced within the brain and they can influence our mood, behavior, and cognitive function. Notably, our gut provides around 95% of our body’s serotonin (3)—a neurotransmitter which plays a crucial role in regulating our mood. Gut bacteria also contribute to the production of dopamine, gamma-aminobutyric acid (GABA) and norepinephrine (4), which regulate pleasure, motivation, and anxiety levels. An imbalance in gut bacteria, or dysbiosis, can disrupt the production of these key neurotransmitters, potentially contributing to the development of mental health conditions.
 Dysbiosis can also cause the intestinal lining to become more permeable, allowing potentially harmful substances to enter the bloodstream and trigger systemic inflammation. Over time, chronic inflammation may contribute to the development of mental health conditions, including depression and anxiety, as it can interfere with normal brain function and neurotransmitter balance (5) One way the gut controls inflammation is through the production of short-chain fatty acids (SCFAs), which are key metabolites produced when gut bacteria ferment dietary fiber. Dysbiosis can reduce the production of SCFAs, such as butyrate and propionate, which help to support the integrity of the blood-brain barrier and intestinal lining by enhancing the integrity of tight junctions.(6,7)
Dysbiosis can also cause the intestinal lining to become more permeable, allowing potentially harmful substances to enter the bloodstream and trigger systemic inflammation. Over time, chronic inflammation may contribute to the development of mental health conditions, including depression and anxiety, as it can interfere with normal brain function and neurotransmitter balance (5) One way the gut controls inflammation is through the production of short-chain fatty acids (SCFAs), which are key metabolites produced when gut bacteria ferment dietary fiber. Dysbiosis can reduce the production of SCFAs, such as butyrate and propionate, which help to support the integrity of the blood-brain barrier and intestinal lining by enhancing the integrity of tight junctions.(6,7)
Microbial Shifts in Anxiety and Depression
Systematic reviews and meta-analyses have consistently reported that individuals with anxiety and depression show altered microbial diversity and composition. For instance, a review of multiple studies published in 2023 found a decrease in the Firmicutes/Bacteroidetes ratio and reductions in levels of beneficial microbes including Faecalibacterium spp., Lachnospira, and Butyricicoccus in individuals with anxiety disorders. These individuals also had an increase in
Lactobacillales, Sellimonas, Streptococcus, Fusobacteria, and certain Bacteroidetes spp. Meanwhile, individuals with depression had elevated levels of Akkermansia, Clostridium_sensu_stricto_1, UBA1819, Prevotella and Klebsiella and reductions in Dialister, Fusicatenibacter, Coprococcus spp., and Lachnospira. Shifts in broader bacterial phyla showed increases in Firmicutes and Actinobacteria, with decreases in Bacteroidetes and Proteobacteria in this subset of patients. (8)
Likewise, another review article published in 2023 described decreases in Clostridia levels and a decreased prevalence of Bacteroides, in patients with major depressive disorder with anxiety. (9) While some studies reviewed in this article reported higher levels of Fusobacterium, Escherichia-Shigella, and Ruminococcus gnavus in patients with generalized anxiety disorder and a reduction in Gemmiger, Ruminococcus, and Veillonella in those with anxiety and depression. Across the reviewed studies, individuals with depression tended to show reductions in Firmicutes, Clostridia, and Coprococcus, while experiencing increases in Actinobacteria, Proteobacteria, and Parabacteroides. Other studies have also reported elevated Akkermansia levels and decreased Faecalibacterium, Butyricicoccus, and Lachnospiraceae, suggesting a shift away from beneficial short-chain fatty acid producer (9).
Modulating the Gut Microbiome to Improve Mental Health
The shifts in microbiome diversity and composition that we discussed above suggest that we may be able to manage mental health conditions such as anxiety and depression by targeting the gut microbiome. By promoting the growth of beneficial bacteria and reducing the abundance of harmful microbes, we could potentially restore balance in the gut, reduce chronic inflammation, optimize the production of neurotransmitters and improve mental well-being.
Personalized nutrition can help us to achieve these goals, by tailoring diet and lifestyle changes to match individual gut microbiome profiles. Microbiome testing can provide insight into a person’s unique microbial composition and identify bacterial imbalances that may contribute to mental health issues. With this information, interventions can be customized to support the growth of beneficial microbes and target those that are out of balance.
Recent studies support the effectiveness of this personalized approach. For example, one study demonstrated the effectiveness of a precision nutrition approach powered by artificial intelligence, which informs tailored food and supplement recommendations. Pilot studies of this approach reported a significant improvement in clinical outcomes for patients with severe
anxiety and depression (10) Another study which focused on older adults showed that a personalized diet based on individual needs helped to reduce depression symptoms and improve quality of life (11) Interestingly, this diet intervention was also associated with significant changes in gut microbiota composition, including an increase in microbial diversity. Similarly, probiotics have shown promising results in reducing symptoms of depression and anxiety, further highlighting the potential of microbiome-targeted therapies in managing mental health conditions (12)
How ENBIOSIS Microbiome Testing Could Change Mental Health Care
In order to make the appropriate diet and lifestyle changes to support mental health, it’s crucial to first understand the unique composition of an individual’s gut microbiome. That’s where ENBIOSIS comes in. By leveraging advanced AI-powered microbiome analysis, ENBIOSIS provides a detailed breakdown of the microbes present within the gut. Our analysis not only identifies key microbial imbalances but also compares these findings against general health parameters, offering deeper insights into the connection between gut health and overall well-being. This information allows us to formulate personalized nutrition and supplement recommendations which can help to restore microbial balance and optimize gut health.
Contact us today to find out more about our AI-driven gut microbiome testing services, or take a look at our website to explore our science-backed approach in greater detail.
Contact usReferences:
1. World Health Organization. (2023). Depression. Retrieved March 18, 2025, from https://www.who.int/news-room/fact-sheets/detail/depression
2. World Health Organization. (2023). Anxiety disorders. Retrieved March 18, 2025, from https://www.who.int/news-room/fact-sheets/detail/anxiety-disorders
3. Appleton, J. (2018). The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integrative Medicine: A Clinician’s Journal, 17(4), 28.
4. T Dicks, L. M. (2022). Gut Bacteria and Neurotransmitters. Microorganisms, 10(9), 1838.
5. Ouabbou, S., He, Y., Butler, K., & Tsuang, M. (2020). Inflammation in Mental Disorders: Is the Microbiota the Missing Link? Neuroscience Bulletin, 36(9), 1071.
6. Shin, Y., Han, S., Kwon, J., Ju, S., Choi, T. G., Kang, I., & Kim, S. S. (2023). Roles of Short-Chain Fatty Acids in Inflammatory Bowel Disease. Nutrients, 15(20), 4466.
7.Silva, Y. P., Bernardi, A., & Frozza, R. L. (2020). The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Frontiers in Endocrinology, 11, 25.
8. Xiong, G., Li, J., Cheng, J., Zhou, D., Wu, X., Huang, Y., Saimaiti, A., Yang, J., Gan, Y., & Li, B. (2023). The Role of Gut Microbiota in Anxiety, Depression, and Other Mental Disorders as Well as the Protective Effects of Dietary Components. Nutrients, 15(14), 3258.
9. Kumar, A., Pramanik, J., Goyal, N., Chauhan, D., Sivamaruthi, B. S., Prajapati, B. G., & Chaiyasut, C. (2023). Gut Microbiota in Anxiety and Depression: Unveiling the Relationships and Management Options. Pharmaceuticals, 16(4), 565.
10. Connell, J., Toma, R., Ho, C. H.-C., et al. (2023). Data-driven precision nutrition improves clinical outcomes and risk scores for IBS, depression, anxiety, and T2D. American Journal of Lifestyle Medicine, OnlineFirst.
11. Magzal, F., Turroni, S., Fabbrini, M., Barone, M., Schorr, A. V., Ofran, A., & Tamir, S. (2023). A personalized diet intervention improves depression symptoms and changes microbiota and metabolite profiles among community-dwelling older adults. Frontiers in Nutrition, 10, 1234549.
12. Asad, A., Kirk, M., Zhu, S., Dong, X., & Gao, M. (2024). Effects of prebiotics and probiotics on symptoms of depression and anxiety in clinically diagnosed samples: Systematic review and meta-analysis of randomized controlled trials. Nutrition Reviews, nuae177