What’s Your Gut Got to Do with Psoriasis?
Psoriasis is a chronic autoimmune skin disorder that causes thick, scaly patches to develop on the skin, typically on the elbows, knees, scalp, and lower back. These patches are usually raised, dry and itchy, and may crack and bleed when severe. Symptoms of the condition can vary in severity and often wax and wane, with flare-ups triggered by factors such as stress, infections, or skin injuries. In addition to skin plaques, some people also experience nail psoriasis, which causes pitting, discoloration, or thickening of the nails. In more severe cases, psoriasis can progress to psoriatic arthritis, an inflammatory joint condition that leads to swelling, stiffness, and pain.
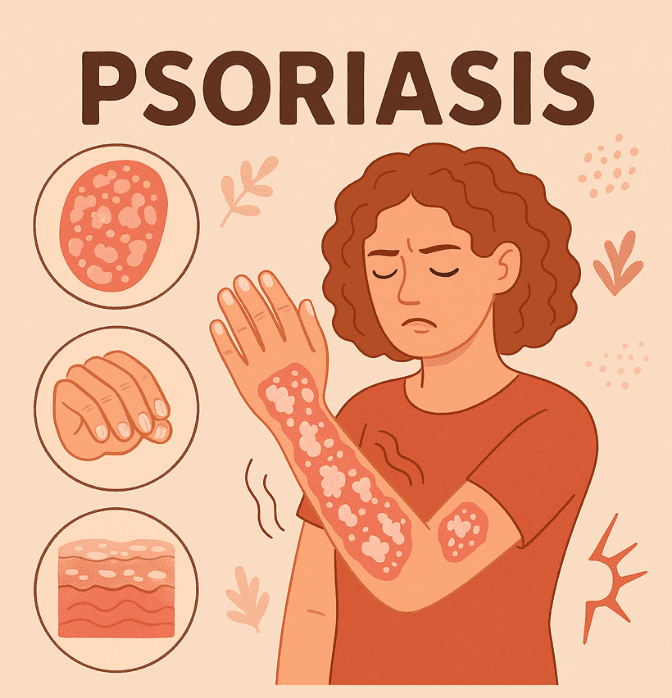 Although it affects the skin, psoriasis is widely recognized as a systemic inflammatory condition that is driven by an overactive immune response. In people with psoriasis, immune cells mistakenly attack healthy skin cells and this triggers inflammation and rapid skin cell turnover. This leads to the buildup of skin cells on the surface, forming the thick, scaly plaques that are characteristic of the condition.
Although it affects the skin, psoriasis is widely recognized as a systemic inflammatory condition that is driven by an overactive immune response. In people with psoriasis, immune cells mistakenly attack healthy skin cells and this triggers inflammation and rapid skin cell turnover. This leads to the buildup of skin cells on the surface, forming the thick, scaly plaques that are characteristic of the condition.
It is estimated that psoriasis affects around 2 to 3% of the global population and it can develop at any age but tends to have two peak periods of onset, with the first between ages 20 and 30 years and the second between 50 and 60 years. While psoriasis is not contagious, the condition can cause significant physical discomfort and emotional distress for those affected. Flare-ups of psoriasis can be painful, disrupt sleeping and even affect confidence if they occur in highly visible places, such as the hands and face.
Psoriasis and the Microbiome: Is the Gut the Real Culprit?
Psoriasis tends to run in families, but exactly how genetics contributes to the condition isn’t fully clear. Increasingly, researchers are turning their focus to the gut microbiome and how it might influence the immune system to trigger or worsen psoriasis. This is because our gut and skin are known to communicate closely through the gut-skin axis, allowing gut bacteria and their metabolites to alter immune responses that affect the skin.
Research increasingly points to distinct gut microbiome patterns in individuals with psoriasis, highlighting shifts in key bacterial groups that are linked to inflammation. For example, studies report an increase in the bacterial group Firmicutes, alongside a decrease in Bacteroidetes compared to healthy controls.,, This shift raises the Firmicutes-to-Bacteroidetes ratio in psoriasis patients, which is often linked to inflammation and changes in metabolic health and immune function. The abundance of Actinobacteria also appears to be altered in psoriasis, although findings are inconsistent, with some studies reporting a decrease in this phylum and others finding it to be elevated.5 This variability highlights the complexity of the gut microbiome in psoriasis and suggests that differences in study populations, methodologies, or disease subtypes might complicate things.
 Proteobacteria is another phylum that shows altered proportions in psoriasis patients. In one particular study, Proteobacteria were found to be significantly increased in individuals with psoriasis compared to healthy controls, alongside an overall reduction in gut microbial diversity. Looking closer at specific bacteria, Faecalibacterium prausnitzii, which is known for its anti-inflammatory effects, has been found to be reduced in psoriasis patients. Similarly, Akkermansia muciniphila and Lachnospira, key butyrate producers, have also been shown to be decreased in those affected. In contrast, Prevotella copri and Parabacteroides merdae were found to be significantly enriched in those with psoriasis compared to healthy controls.6
Proteobacteria is another phylum that shows altered proportions in psoriasis patients. In one particular study, Proteobacteria were found to be significantly increased in individuals with psoriasis compared to healthy controls, alongside an overall reduction in gut microbial diversity. Looking closer at specific bacteria, Faecalibacterium prausnitzii, which is known for its anti-inflammatory effects, has been found to be reduced in psoriasis patients. Similarly, Akkermansia muciniphila and Lachnospira, key butyrate producers, have also been shown to be decreased in those affected. In contrast, Prevotella copri and Parabacteroides merdae were found to be significantly enriched in those with psoriasis compared to healthy controls.6
Lastly, increases in bacteria that have been associated with inflammation, such as Escherichia coli7, Megasphaera elsdenii and Eubacterium CAG 180 have also been observed, mirroring patterns seen in other inflammatory diseases.
Together, these microbial shifts suggest that psoriasis is linked to gut dysbiosis characterized by reduced diversity and an imbalance favoring bacteria that may promote inflammation. This disturbed gut environment likely contributes to the immune system dysfunction that is seen in psoriasis patients, making the gut microbiome a promising target for future therapies.
Can Lifestyle Changes Improve Psoriasis Symptoms?
So, can we actually improve psoriasis symptoms by altering the bacteria that are present in our gut? The science suggests that we can. A newly published review highlights how existing psoriasis treatments, including biologics and narrow-band UVB therapy, can influence the composition of the gut microbiome. These therapies appear to shift gut bacteria toward a less inflammatory balance, which may help to explain part of their effectiveness. This growing evidence suggests that the gut microbiome can indeed play an important role in psoriasis and its treatment. Alongside treatment, lifestyle interventions can positively influence the gut microbiome, helping to reduce systemic inflammation and improve immune function. Diet changes have been shown
to improve psoriasis symptoms by restoring a healthier gut bacteria balance. For instance, adherence to a Mediterranean Diet has been linked to beneficial shifts in the microbiome that may lower disease severity. While a gluten-free diet may improve symptoms in patients who have gluten sensitivity or celiac disease, alongside their psoriasis.
Meanwhile, probiotics are also emerging as a promising complementary approach to the treatment of psoriasis. Studies have found that certain probiotic strains can reduce inflammation and improve psoriasis symptoms by modulating the gut microbiome. For example, psoriasis patients taking the oral probiotic Bifidobacteria infantis 35624 for 6 to 8 weeks experienced a reduction in systemic inflammation markers, including C-reactive protein (CRP) and the pro-inflammatory cytokine TNF-α. Likewise, patients with plaque psoriasis who received a probiotic mixture over 12 weeks showed significant improvement in their Psoriasis Area and Severity Index (PASI) and had a lower risk of relapse after finishing the treatment. In this case, gut microbiome analysis confirmed that the probiotic mixture had reshaped their bacterial communities.
Given how individual our microbiomes are, a personalized approach combining targeted nutrition, prebiotics, and probiotics offers a promising way of supporting existing treatments and optimizing psoriasis management.
Harnessing the Science of the Microbiome to Improve Psoriasis

At Enbiosis, we take the guesswork out of gut health. Our advanced AI-powered microbiome analysis allows us to provide personalized nutritional recommendations designed to rebalance your gut microbiota and reduce inflammation. By understanding the unique composition of your gut microbiome, we can identify imbalances and tailor interventions that work with the body.
Our client from the UK shared a powerful update: after living with psoriasis for 15 years, their symptoms cleared within just 4 months of starting Enbiosis’ personalized microbiome modulation protocol. This real-world feedback reinforces the science behind our gut-skin axis approach and highlights the potential of targeting the microbiome to manage chronic inflammatory conditions like psoriasis. We’re proud to be part of such life-changing transformations.
Visit our website to discover more about our science-backed approach to improving gut health and managing psoriasis, or contact us to find out how we can help.
References:
1 National Psoriasis Foundation. (2022). Psoriasis statistics. Retrieved May 19, 2025, from https://www.psoriasis.org/psoriasis-statistics/
2 Chen, Y. J., Ho, H. J., Tseng, C. H., Lai, Z. L., Shieh, J. J., & Wu, C. Y. (2018). Intestinal microbiota profiling and predicted metabolic dysregulation in psoriasis patients. Experimental Dermatology, 27(12), 1336–1343.
3 Shapiro, J., Cohen, N. A., Shalev, V., Uzan, A., Koren, O., & Maharshak, N. (2019). Psoriatic patients have a distinct structural and functional fecal microbiota compared with controls. The Journal of Dermatology, 46(7), 595–603.
4 Dei-Cas, I., Giliberto, F., Luce, L., Dopazo, H., & Penas-Steinhardt, A. (2020). Metagenomic analysis of gut microbiota in non-treated plaque psoriasis patients stratified by disease severity: Development of a new Psoriasis-Microbiome Index. Scientific Reports, 10(1), 1–11.
5 Gao, Y., Lou, Y., Hui, Y., Chen, H., Sang, H., & Liu, F. (2025). Characterization of the Gut Microbiota in Patients with Psoriasis: A Systematic Review. Pathogens, 14(4), 358.
6 Xiao, Y., Jing, D., Xiao, H., Mao, M., Kuang, Y., Shen, M., Lv, C., Jian, X., Peng, C., & Chen, X. (2025). Metagenomics Analysis of Altered Gut Microbiome in Psoriasis and the Mediation Analysis: A Case-Control Study. Psoriasis: Targets and Therapy, 15, 45.
7 Eppinga, H., Sperna Weiland, C. J., Thio, H. B., Janneke, C., Nijsten, T. E., Peppelenbosch, M. P., & Konstantinov, S. R. (2016). Similar Depletion of Protective Faecalibacterium prausnitzii in Psoriasis and Inflammatory Bowel Disease, but not in Hidradenitis Suppurativa. Journal of Crohn’s and Colitis, 10(9), 1067–1075.
8 Tan, L., Zhao, S., Zhu, W., Wu, L., Li, J., Shen, M., Lei, L., Chen, X., & Peng, C. (2018). The Akkermansia muciniphila is a gut microbiota signature in psoriasis. Experimental Dermatology, 27(2), 144–149.
9 Buhaș, M. C., Gavrilaș, L. I., Candrea, R., Cătinean, A., Mocan, A., Miere, D., & Tătaru, A. (2022). Gut Microbiota in Psoriasis. Nutrients, 14(14), 2970.
10 Memariani, M., & Memariani, H. (2025). New horizons in the treatment of psoriasis: Modulation of gut microbiome. Heliyon, 11(1), e41672.
11 Kranyak, A., Haran, K., Smith, P., Johnson, C., Liao, W., & Bhutani, T. (2024). The Mediterranean Diet as a Potential Solution to the Gut Microbiome Dysbiosis in Psoriasis Patients. Journal of Psoriasis and Psoriatic Arthritis, 9(2), 69–81.
12 Michaëlsson, G., Gerdén, B., Hagforsen, E., Nilsson, B., Kraaz, W., Hjelmquist, G., & Lööf, L. (2000). Psoriasis patients with antibodies to gliadin can be improved by a gluten-free diet. British Journal of Dermatology, 142(1), 44–51.
13 Groeger, D., O’Mahony, L., Murphy, E. F., Bourke, J. F., Dinan, T. G., Kiely, B., Shanahan, F., & Quigley, E. M. (2013). Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut. Gut Microbes, 4(4), 325–339.
14 Navarro-López, V., Martínez-Andrés, A., Ramírez-Boscá, A., Ruzafa-Costas, B., Núñez-Delegido, E., Carrión-Gutiérrez, M. A., … Chumillas-Lidón, S. (2019). Efficacy and Safety of Oral Administration of a Mixture of Probiotic Strains in Patients with Psoriasis: A Randomized Controlled Clinical Trial. Acta Dermato-Venereologica, 99(12), 1078–1084.